Healthcare construction means building medical facilities that meet strict safety and care standards. Learn key steps, costs, and how to manage every challenge.

Use this FREE Project Cost Dashboard to monitor budgets, actuals, forecasts, and cost variances at a glance. Track your project’s financial health in one clear, easy-to-read view.

Healthcare construction is one of the most complex sectors in the building industry. Unlike other projects, it directly impacts medical safety, patient outcomes, and how healthcare professionals deliver care. It involves strict regulations, live clinical environments, and coordination across many disciplines.
Let’s talk about what sets healthcare construction apart and what it takes to get it right. You’ll learn key hospital construction phases, common challenges, and solutions to deliver safe, future-ready medical facilities.
Healthcare construction involves the planning, design, and construction or renovation of healthcare facilities. It includes everything from structural work to interior spaces like operating theatres, imaging rooms, and outpatient areas. These projects are highly specialized and change often with advances in medical technology.
Because health is the priority, every part of a healthcare build needs to support patient safety, staff workflows, and clinical care. That means planning for strict infection control, essential services, like medical gases and HVAC, and designs that support how care is delivered.
Healthcare construction includes facilities built to deliver medical care, support patient health, and meet strict clinical and safety standards. These projects are purpose-built to serve different types of treatment, diagnostics, and care delivery.
Here are common examples of healthcare construction projects and what they typically involve:
One example of a successful healthcare construction project is the Cedars-Sinai Pavilion in Los Angeles, a multi-level expansion designed with prefabricated MEP systems and smart building technologies.
Another is Stanford Hospital in Palo Alto, built with seismic resilience and full BIM integration to support long-term flexibility and complex clinical operations.

Healthcare construction involves strict clinical, safety, and technical requirements that don’t apply to standard commercial construction. Every decision must support patient care, infection control, and long-term facility performance.
✅ Clinical Needs Drive the Design
Construction drawings must reflect clinical workflows. Medical teams review everything from scrub room placement to patient transport routes. Designs must also meet infection control and operational standards before construction starts.
✅ Built for the Future
Hospitals and clinics must support changing models of care, like telehealth or same-day surgery. Projects need scalable infrastructure, like extra risers, ceiling space, and structural load capacity, for future upgrades without major rebuilds.
✅ Infection Control Starts at Design
Pressurized rooms, clean/dirty zoning, and antimicrobial finishes are essential. Construction teams must also plan for how infection control will be maintained during works, especially in live facilities.
✅ Redundancy and Risk Management
Critical healthcare systems, like power, oxygen, and water, must have backups. Healthcare projects often require dual power feeds, emergency generators, and fail-safes built into all essential services. This level of resilience adds layers to engineering, testing, and certification.
✅ Tight Staging and Commissioning
Projects are often staged in phases to keep parts of a hospital operational. This means multiple handovers, interim certifications, and extra coordination between teams. Final commissioning includes not just building systems but also clinical simulations and equipment testing.
✅ Higher Compliance Burden
In addition to local building codes, healthcare buildings must meet health-specific guidelines (like AHFG or FGI), infection control policies, and equipment supplier requirements. Design teams must provide extensive documentation for accreditation and facility licensing.
✅ Specialized Materials and Equipment Requirements
Healthcare facilities use materials that reduce infection risks and withstand constant cleaning. Equipment like MRI machines and surgical lights comes with strict spatial, structural, and shielding needs that must be factored into the design and construction early.

The healthcare sector is shifting fast. Design and delivery methods in healthcare facility construction now respond to environmental goals, digital health needs, and the push for faster, more flexible builds, especially outside major cities.
Modular builds use pre-assembled rooms or components, built off-site and installed quickly. Prefab is common in temporary wards, clinics, and diagnostic spaces. It reduces site disruption, shortens build time, and improves quality control. Hospitals use it to expand without shutting down healthcare services or delaying care.
Hospitals are major energy users. Net-zero targets push designers to reduce emissions through passive design, solar power, energy-efficient HVAC, and smart controls. Many new builds aim for Green Star or LEED ratings. Sustainability cuts operating costs and improves air quality for patients and staff.
Smart hospitals integrate systems for lighting, HVAC, access control, and patient monitoring. Healthcare designs now include infrastructure for telehealth, real-time locating systems (RTLS), and digital wayfinding. Coordinating IT and clinical tech from the start is key to avoiding retrofits or tech clashes after handover.
Healthcare is shifting closer to home. Post-COVID, governments are funding more local health hubs, day surgeries, children's hospitals, and outpatient clinics in outer metro and rural areas. These builds focus on access, speed, and flexible spaces. They often use prefab and fast-tracked models to meet urgent care needs with smaller footprints.
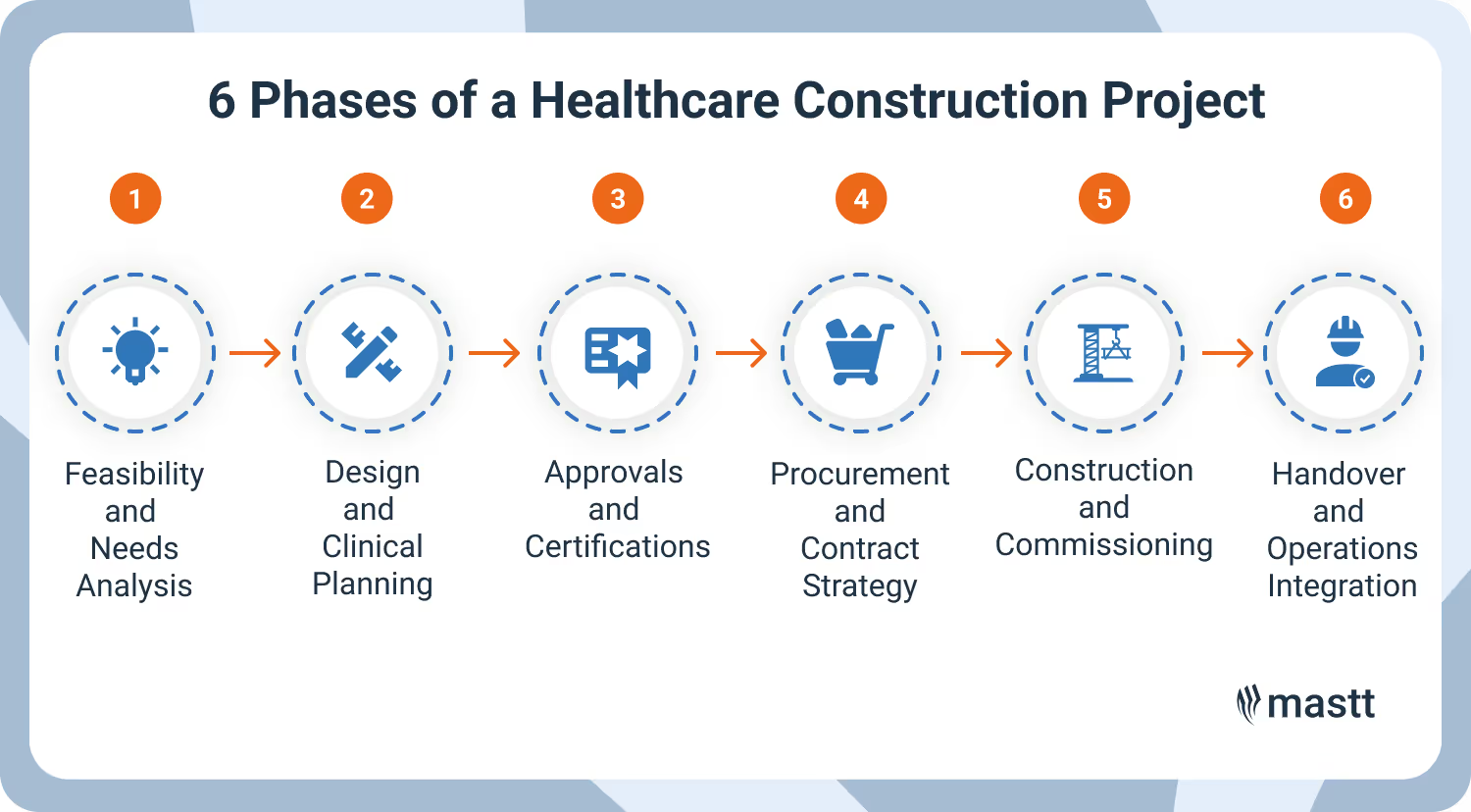
A healthcare construction project moves through six critical phases. Each step involves specific clinical, regulatory, and technical tasks that affect how the facility will function once open. What makes this process unique is the constant need to align design and delivery with patient care.
Here’s how the full healthcare construction process works.
This phase tests whether the project is viable. Health departments, project owners, and planners define what services are needed, who the facility will serve, and how many beds, clinics, or imaging rooms are required.
The team studies population health data, service catchment gaps, site suitability, and existing infrastructure. They check if the site supports clinical access, ambulance movements, infection zoning, and future expansion. Early estimates outline size, cost, and staging needs.
At this point, it’s common to engage a healthcare planner or project manager to help assess risk, develop a master plan, and flag potential delays tied to services, heritage overlays, or planning restrictions.
Design starts with clinical vision. The team holds user group workshops with nurses, doctors, facilities staff, and infection control leads. These sessions define room functions, flows, adjacencies, and clinical dependencies.
Design moves through construction design phases:
During this phase, the healthcare design must meet national guidelines (like AHFG or FGI) and healthcare engineering codes. The team also plans for medical equipment placement, radiation shielding, fire egress, and ICT integration.
Health projects face multiple layers of approval. Plans are submitted to:
Depending on scope, the process may require staged submissions for early works, services, and final design. Hospital construction often need staged occupancy certificates tied to commissioning and handover milestones.
Delays in approvals can stall procurement and push back construction, so teams typically map out all submission dates in detail.
Construction procurement in the healthcare industry must balance price, risk, and flexibility. Project owners choose a delivery model based on complexity and timelines.
Procurement involves:
Healthcare procurement must factor in hospital commissioning dates, government funding cycles, and any staged works that affect operations.
Once approvals are in place, site works begin. If building within a live facility, medical construction zones must be sealed off and access controlled. HEPA filtration, noise buffers, and after-hours work are common in operational hospitals.
Work typically follows this sequence:
Commissioning covers everything from switchboard tests to nurse call checks. Hospitals also conduct clinical simulations to validate workflows, zoning, and emergency procedures before occupation.
Handover happens in stages, sometimes by floor, wing, or service zone. Operations teams inspect and sign off on rooms, systems, and documents. Staff are trained on new layouts, systems, and safety protocols.
Key steps:
Post-handover, some teams stay on for defect management, move-in coordination, or Stage 2 works. A successful handover means clinical teams can deliver care safely from day one, with no surprises.
Healthcare construction brings together clinical, technical, and construction teams, all with distinct roles. Success depends on clear responsibilities, constant communication, and early input from the right people.
Each role brings essential expertise. For example, when designing an ICU, architects draft the layout, engineers map out services like oxygen and power, and clinical staff review visibility lines and workflow. The project manager pulls it all together, coordinating input, resolving conflicts, and keeping everything on schedule.
Healthcare projects use different project delivery methods depending on their risk, complexity, and funding structure. Each method affects how teams work together, how fast you can build, and how much control the owner keeps.
In design and construct, the builder takes on both design and construction under one contract. This gives cost certainty early and speeds up delivery. But it limits design flexibility and may reduce clinical input if not managed carefully. Best for straightforward scopes with tight budgets and timelines.
The managing contractor oversees design and construction, but subcontracts trade packages on the client’s behalf. This gives the client more control over design, trade selection, and scope changes. It suits large public hospital projects with staged delivery or complex staging needs.
The builder is engaged early, often during concept or schematic design, to give input on buildability, staging, and costs. The contract can later be converted to D&C or another form. Early contractor involvement works well for projects with high staging risk, complex services, or fast-track goals.
All parties, including the client, builder, and consultants, work under a shared contract with shared risk and reward. There’s no blame clause. Alliancing supports transparency, strong collaboration, and flexible scope evolution. It fits large, high-risk projects where stakeholder input must drive every decision.
In public-private partnerships, a private consortium designs, builds, finances, and operates the facility for a defined term. This suits major state hospital projects with long-term service contracts (e.g. maintenance, cleaning). It requires detailed scoping, legal frameworks, and high commercial expertise from the owner.
Healthcare construction costs vary widely depending on facility type, location, complexity, and level of specialized services. Costs can range from $500 to over $1,500 per square foot in the U.S., with urban projects typically more expensive than regional builds.
Note: These figures reflect base construction costs and don’t include land, equipment, or ongoing operational fitout. Hospitals and diagnostic centers often cost more due to strict clinical standards, advanced MEP systems, and compliance requirements.
Healthcare construction comes with more risk, more oversight, and less room for error than most other project types. Each challenge affects time, cost, and safety, often all at once.
Here are the common healthcare construction challenges and how to solve them:
⚠️ Tight Schedules
Healthcare projects often face fixed deadlines. These can come from government funding cycles, urgent service needs, or clinical commissioning dates. Delays can disrupt planned openings or force temporary workarounds that add cost and risk. Fast-tracking must still meet clinical and compliance standards, leaving little room for error.
💡 Solution: Lock in critical path items early. Use fast-track strategies like early works packages or modular construction. Track milestones closely and involve clinical teams in schedule reviews to avoid late surprises.
⚠️ Budget Pressure
Most healthcare projects rely on public or non-profit funding. Budgets are set early and leave little contingency. Rising material costs, complex service scopes, and equipment requirements can quickly blow past estimates. Value management is essential. But cost cuts must never compromise patient experience or long-term performance.
💡 Solution: Set a realistic cost baseline with escalation allowances and clear exclusions. Run early value engineering workshops with clinical input to protect critical scope. Track forecast costs in real time, not just monthly.
⚠️ Stakeholder Complexity
Dozens of voices shape a healthcare project, including healthcare organizations, healthcare clients, facilities managers, health department reps, and executive boards. Each group has different needs. Balancing these takes strong leadership, clear documentation, and constant communication. Misalignment here can trigger late design changes, user dissatisfaction, or regulatory pushback.
💡 Solution: Use a structured stakeholder map and formal engagement plan. Lock in decision timelines for user groups. Assign a dedicated stakeholder manager to bridge communication between healthcare and construction professionals and capture critical feedback early.
⚠️ Regulatory Red Tape
Approvals go beyond standard planning and building permits. Health projects often need sign-off from multiple agencies: health departments, infection control, fire safety, building certifiers, and more. Each submission must meet detailed guidelines and may require resubmissions or staged approvals. Tracking these timelines is critical to avoid delays.
💡 Solution: Build a detailed approvals tracker into the project schedule. Submit documentation in stages to avoid bottlenecks. Involve certifiers and health reps early during design to spot compliance risks before submission.
⚠️ Operational Continuity
Construction often happens in or next to active hospitals or clinics. Builders must protect patients and medical staff from dust, noise, vibration, and access changes. Shift work, HEPA-filtered zones, and strict staging plans are common. A single misstep, like blocking emergency routes or disrupting power, can put lives at risk.
💡 Solution: Develop a staging and impact management plan with hospital operations teams. Use temporary partitions, off-hours work, and vibration monitoring. Assign a live environment coordinator to manage disruptions daily and respond quickly when issues arise.
Healthcare projects demand speed, precision, and constant coordination, especially when working in live environments or under strict compliance timelines. Mastt helps project managers and owners stay in control with real-time data, easy reporting, and tools built for capital works.
Here’s what Mastt brings to your healthcare construction program:
Healthcare projects are complex, and even small delays can impact patient care. Mastt keeps everything on track by turning project data into clear insights. So you can make fast decisions, avoid surprises, and deliver facilities that open on time and are ready for care.
Healthcare construction is about delivering safe, functional spaces that support patients, staff, and clinical outcomes from day one. That means designing with intent, managing risks early, and keeping teams aligned every step of the way.
Healthcare construction success comes from getting the details right: infection control, services coordination, clinical input, and real-time reporting. When you build with care at the core, you deliver spaces that are ready to heal.

Cut the stress of showing up unprepared
Start for FreeTrusted by the bold, the brave, and the brilliant to deliver the future